The endoscopy service at Salford Royal performs approximately 7,000-8,000 procedures a year.
Endoscopy not only helps diagnose the underlying cause for bowel and stomach related symptoms but is increasingly used to provide treatment for a range of conditions which can be treated as part of the procedure. We also provide complex therapeutic procedures including ERCP, EUS/FNA, EMR and ESD within our Endoscopy department.
We are proud to support services for specialist Upper Gastrointestinal conditions as Salford is the centre for Upper gastrointestinal cancers in greater Manchester.
We take pride in treating each of our patients with respect and providing the best possible care every time. We consistently receive excellent feedback for the quality of our service and work with our patients to identify ways to further improve our service.
We provide daily planned lists where patients are invited to attend for a procedure which often doesn’t require admission to hospital. We also perform urgent procedures for patients who are already admitted to hospital.
The organisation operates an out of hours on call system where a consultant endoscopist is always available to perform emergency procedures for any patients who required such lifesaving procedures.
The endoscopy unit provides an excellent endoscopy training program and consistently receives excellent feedback from both medical and surgical trainees. We also provide excellent training for nursing and admin staff at our endoscopy unit.
Endoscopy is a procedure where a thin flexible tube is used to view the inside of Gastrointestinal Tract to help diagnosis and treat a range of gastrointestinal conditions.
Increasingly we can perform procedures which previously required surgery to treat. We can perform treatment for GI bleeding, Polypectomy, removal of large and complex polyps using EMR/ESD techniques, Palliation of cancer including insertion of stents, removal of stones from Common bile duct (Gall bladder tube), dilatation (stretching) of strictures (narrowing) to name but a few.
Endoscopy is a safe procedure and often performed with local spray or sedation, the majority of patients go home a few hours after recovery and receive a diagnosis and treatment plan for their conditions during their visit.
The range of procedures we perform at our hospitals include:
- Gastroscopy
- Flexible Sigmoidoscopy
- Colonoscopy
- Endoscopic Retrograde Cholangiopancreatography (ERCP)
- Endoscopic ultrasound/fine needle aspiration (EUS/FNA)
- Endoscopic submucosal dissection (ESD)
- Radiofrequency ablation (RFA/HALO)
- Upper Gastrointestinal stent insertion
- Percutaneous endoscopic gastrostomy (PEG) and other feeding tubes.
- Colon Capsule
General Endoscopy enquires – 0161 206 5959
Booking Team (for cancelations or amendments to appointments) – 0161 778 5402
Medication enquires – 0161 206 5958
Bowel Preparation enquires – 0161 206 5237
Service Team – 0161 206 7677
Out of Hours Emergency advice (after 17:00hrs, 7 days a week) – 0161 206 4848
Procedures
What is a colonoscopy?
Your doctor has advised that you should have a colonoscopy. This is a complete examination of your large bowel (otherwise known as the large intestine or the colon).
This investigation is performed using an instrument called a colonoscope. It is a long flexible tube about the same thickness as your little finger. The colonoscope lights up the lining of your large bowel and has a sensor on the end to capture video images which are relayed back to a television screen in the endoscopy room.
During the investigation, the endoscopist may need to take some tissue samples, known as biopsies, from the lining of large bowel for further analysis. This is completely painless. Photographs may also be taken for your medical records.
Why do I need to have a colonoscopy?
You have been advised to undergo this test in order to try to find the cause of your symptoms, help with treatment and, if necessary, to decide on further investigations.
There are many reasons why this colonoscopy may be recommended and your doctor will have discussed these with you.
Common indications for a colonoscopy include:
- A change in your usual bowel habit to constipation or diarrhoea
- Bleeding from the back passage
- To find the cause of anaemia
- To review a known bowel condition (e.g. inflammatory bowel disease, colonic polyps)
- To assess or treat an abnormality seen on other tests such as barium enema or CT scan
- A strong family history of bowel cancer
- As part of the national bowel cancer screening program
If none of these apply to you, your doctor will explain any other reasons there may be for having this test.
Will I receive sedation?
It is important that you are comfortable during the procedure to ensure that the endoscopist can perform the procedure successfully.
It is usual for most people to have a sedative drugs and a painkiller to be administered into a vein in your arm which will make you drowsy and relaxed for the colonoscopy. This is known as intravenous sedation.
Alternatively, we can give you Entonox gas during the procedure which will help to ease any pain or discomfort and has a calming effect.

Sedative drugs can be administered into a vein in your arm which will make you drowsy and relaxed for the gastroscopy.
These drugs will NOT make you unconscious like a general anaesthetic. You will be in a state known as cooperative sedation, which means that, although drowsy, you will still be able to hear what is said to you and will be able to follow simple instructions during the investigation, sometimes sedation can also prevent you from remembering anything about the procedure afterwards.
Your oxygen levels and heart rate will be monitored during the procedure, and your blood pressure may also be recorded. You will receive oxygen by small tubes which rest just below your nose.
If you choose to have sedation, you must arrange for a friend or relative to collect you from the Endoscopy Unit and we recommend that they stay with you afterwards. You must not drive, ride a bike, operate machinery, climb ladders, or sign important documents for 24 hours following sedation.
If you are not able to make these arrangements, we will not be able to give you sedation.
Entonox gas 
Entonox is a colourless and odourless gas comprised of oxygen and nitrous oxide (commonly known as laughing gas). It is the same gas used by pregnant women during labour pains. It can also be beneficial during flexible sigmoidoscopy and colonoscopy because it helps to relieve pain and has a calming effect.
The gas is administered by a special mouth-piece which you will be asked to hold yourself during the procedure. A two-way valve system allows you to breathe normally through the mouth-piece. The Entonox gas begins to work within 30 seconds and you may feel slightly light headed and sleepy. You can control the amount of gas that you receive yourself by simply removing the mouth-piece but your nurse will monitor you closely throughout the procedure.
One of the benefits of Entonox is that once your procedure is over, the gas is rapidly eliminated from the body and you are usually safe to leave the department soon afterwards. Unlike with intravenous sedation, you are permitted to drive just 30 minutes after the test as long as you feel back to your normal self.
Entonox is very safe in the majority of people. It can cause mild nausea, dizziness and a dry mouth. As the effects of the drug wear off very quickly, so do these side effects. Please be aware that Entonox may not be suitable for you if you have respiratory conditions such as COPD, severe bullous emphysema or a collapsed lung.
Some patients choose to undergo colonoscopy without any drugs but for many people the test can become very uncomfortable and occasionally intolerable in this situation.
How to prepare for your colonoscopy
It is extremely important that your bowel is completely empty before a colonoscopy to allow adequate inspection of the lining of your colon, this is usually achieved by giving you a bowel cleansing laxative to take at home on the day before your procedure. Sometimes, an enema on the day of the test is all that is required, you will be informed if this is the case
At our Endoscopy units we usually use a bowel cleansing agent called Moviprep®, you should have been provided with this medication along with clear instructions on how to administer it. If you have any queries do not hesitate to contact the endoscopy unit and we will be happy to help you.
What happens when I arrive?
Our reception staff will greet you on the unit; once they have checked your details you will be offered a seat in the waiting room. Your named nurse will ask you to come through to the preparation area shortly before your procedure.
Your Nurse will check your identity and go through any medical conditions, medication and allergies to ensure it is safe to proceed. It would be very helpful if you could bring a list of all your medication with you, your Nurse will also ensure arrangements have been made for your journey home. Your blood pressure and pulse will be checked prior to the procedure.
You will be asked to change into a hospital gown and we can also provide modesty shorts which keep you well covered during the procedure to preserve your dignity.
Please do not bring large amounts of money or valuables with you.
Your Endoscopist will go through your consent form and answer any questions you may have. If you have already signed your consent form, we will confirm that you have not changed your mind.
If you have decided to have sedation, a plastic tube, known as a cannula will be inserted into a vein in your hand or arm to allow the drugs to be injected.
What happens during the procedure?
The colonoscope is introduced into the back passage and maneuvered around the entire length of your large bowel and in some cases into the end portion of your small bowel known as the terminal ileum. There are some bends that naturally occur in the bowel and negotiating these may be uncomfortable for a short period of time but the sedation and analgesia will minimise any pain.
Air is gently passed into the bowel during the investigation to facilitate the passage of the colonoscope. You may be asked to change position during the test, to help pass the colonoscope around your bowel, and the endoscopy nurses will help you move if necessary.
We will ensure that you are well covered up throughout the procedure to preserve your dignity.
Once the colonoscope has been passed all the way around your bowel, the endoscopist will slowly withdraw the instrument making a close inspection of the lining of your bowel to look for any abnormalities. Some of the air blown into the bowel will be removed as well, which will ensure you remain comfortable.
During the procedure samples may be taken from the lining of your bowel, known as biopsies for analysis in our laboratories. These will be retained for future tests if they become necessary.
The whole procedure usually takes between 20 and 30 minutes but can be very variable depending on how curved your bowel is and whether any additional procedures such as polypectomy are required.
What is a polyp/polypectomy?
A polyp is a small growth that can form on the lining of the bowel. Most polyps are harmless but if they are left to grow, some forms of polyps can develop in to a cancer.
The removal of a polyp is called a polypectomy and is performed by using a variety of instruments through central channels of the endoscope.
What happens after the procedure?
You will be escorted to the recovery area in order to rest while you recover from your procedure, if you chose to have throat spray, you will be offered a cold drink when the sensation in your throat has returned to normal.
If you have received sedation, it usually takes about 30 minutes for the initial effects of sedation to wear off although some people may feel fully alert immediately after the procedure, while you recover your oxygen levels, blood pressure and heart rate will be monitored. However, the drugs remain in your blood system for up to 24 hours and you can intermittently feel drowsy with lapses of memory. You will need someone to escort you home and supervise you for this 24 hour period.
If you received Entonox gas during the procedure, its effects usually wear off within a few minutes. You will be observed in the department until you feel back to your normal self.
Before you leave the department, your nurse or doctor will explain the findings of your gastroscopy and any medication or further investigations that may be needed; they will also inform you if you require further appointments.
If biopsies were taken, they will need to be sent to the pathology lab for further analysis. It may take up to a fortnight for these results to be available, a copy of the results will be sent to your GP.
Sedation can make you forgetful and you may like to have a family member or friend with you when you are given this information.
Are there any risks?
A Colonoscopy is generally regarded as a very safe test, however as with most medical procedures, there are some risks involved. Your doctor will have considered these risks and felt that the benefits of this procedure outweigh the potential risks before they suggested that you should have it carried out.
- You may experience bloating and abdominal discomfort for a few hours after the procedure because air is used to inflate the stomach. This can often be relieved by belching.
- If you choose to have sedative drugs, these can cause your breathing to slow down or result in a fall in your blood pressure. This is the reason we do not give high doses of the drugs for the procedure. We monitor your breathing and oxygen levels carefully throughout and this rarely becomes a problem. In any case, an antidote to the sedative drugs that we use is always available and this can reverse its effects immediately.
- There is a risk of causing bleeding at the site of biopsies, but this is uncommon, usually minor, and usually stops on its own. Rarely, bleeding may necessitate a blood transfusion or further procedures to stop the bleeding.
- There is a risk of causing a tear (otherwise known as a perforation) with the telescope. This risk is very small and can occur in 1 in 1,000 cases.
- Colonoscopy is not a perfect test, whilst we normally will get excellent views, there is a small risk (between 5-10%) that we can miss pathology during your procedure due to the number of bends and folds that are in the bowel and the quality of the bowel preparation. You will be advised that if your symptoms persist or if you develop any new symptoms, you should seek medical advice.
If the bowel preparation has not been effective and there is still stool in your bowel we may need to rebook your procedure with a different bowel preparation.
If you are worried about any of these risks, please speak to your doctor or a member of the team before your test.
Are there any alternatives?
An X-ray test (barium enema) or a CT scan (CT virtual colonoscopy) can be used to look at your large bowel, the main drawback of these tests is that they only provide pictures of the shape of your bowel and do not allow samples to be taken or any polyps to be removed. You would require a similar bowel preparation for these tests as well.
Your doctor will have considered a barium enema or CT virtual colonoscopy for you before asking you to have a flexible sigmoidoscopy.
If you do have questions about these alternatives, please mention them to your doctor.
What is a gastroscopy?
This is an examination of your oesophagus (gullet or foodpipe), stomach and the first part of your small bowel called the duodenum.
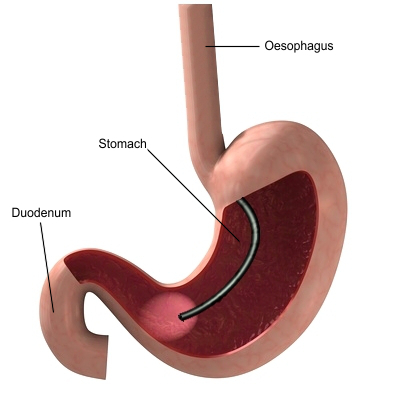
The instrument used for this investigation is called a gastroscope. It is a flexible tube with a diameter less than that of your little finger. The gastroscope lights up the lining of your upper digestive tract and has a sensor on the end to capture video images which are relayed back to a television screen.
During the investigation, the endoscopist may need to take some tissue samples known as biopsies from the lining of your upper digestive tract for further analysis. This is completely painless. The samples may be retained for further tests. Photographs may be taken for your medical records
Why do I need to have a gastroscopy?
You have been advised to undergo this investigation to find the cause for your symptoms, help with treatment and if necessary, to decide on further investigation.
There are many reasons for this investigation including:
- Indigestion
- Anaemia
- Weight loss
- Vomiting
- Passing black motions
- Vomiting blood
- Difficulty swallowing
It is important that you are comfortable during the procedure to ensure that the endoscopist can perform the procedure successfully.
Will I have sedation or throat spray?
You can choose from the following options to help you remain comfortable for the test:
1. Intravenous sedation

Sedative drugs can be administered into a vein in your arm which will make you drowsy and relaxed for the gastroscopy.
These drugs will NOT make you unconscious like a general anaesthetic. You will be in a state known as cooperative sedation, which means that, although drowsy, you will still be able to hear what is said to you and will be able to follow simple instructions during the investigation, sometimes sedation can also prevent you from remembering anything about the procedure afterwards.
Your oxygen levels and heart rate will be monitored during the procedure, and your blood pressure may also be recorded. You will receive oxygen by small tubes which rest just below your nose.
Important reminder: If you choose to have sedation, you must arrange for a friend or relative to collect you from the Endoscopy Unit and we recommend that they stay with you afterwards. You must not drive, ride a bike, operate machinery, climb ladders, or sign important documents for 24 hours following sedation. If you are not able to make these arrangements, we will not be able to give you sedation.
2. Local anaesthetic throat spray
A local anaesthetic drug (lignocaine or xylocaine) is sprayed into the back of the throat to make it numb. It can taste very bitter but works rapidly. It has a similar effect to a dental injection and allows the camera to pass through your throat without you feeling it.
The benefit of choosing throat spray is that you are fully conscious during the gastroscopy, you can go home unaccompanied almost immediately after the procedure and you are permitted to drive. However, you must not have anything to eat or drink until the sensation in your mouth and throat has returned to normal. This usually takes up to 1 hour.
How to prepare for your gastroscopy?
Do not have anything to eat for at least six hours before the procedure, small sips of water can be taken until two hours before your appointment time. This ensures that your stomach is empty and the doctor has a clear view during the test
What happens when I arrive?
Our reception staff will greet you on the unit; once they have checked your details you will be offered a seat in the waiting room. Your named nurse will ask you to come through to the preparation area shortly before your procedure.
Your Nurse will check your identity and go through any medical conditions, medication and allergies to ensure it is safe to proceed. It would be very helpful if you could bring a list of all your medication with you, your Nurse will also ensure arrangements have been made for your journey home. Your blood pressure and pulse will be checked prior to the procedure.
You will be asked to remove any tight clothing, ties, dentures and spectacles. Please do not bring large amounts of money or valuables with you.
Your Endoscopist will go through your consent form and answer any questions you may have. If you have already signed your consent form, we will confirm that you have not changed your mind.
If you have decided to have sedation, a plastic tube, known as a cannula will be inserted into a vein in your hand or arm to allow the drugs to be injected.
What happens during the procedure?
A gastroscopy usually takes 5 to10 minutes but may take longer if further procedures are required. The Endoscopist will place the gastroscope into your mouth and ask you to take a big swallow when it is at the back of your throat, they will then ease the gastroscope carefully down your oesophagus, into your stomach and then into your duodenum.
Your windpipe is deliberately avoided and your breathing will be unhindered.
Any secretions produced during the investigation will be removed using a small suction tube, rather like the one used at the dentist.
Biopsies and photographs may be taken during the procedure.
What happens after the procedure?
You will be escorted to the recovery area in order to rest while you recover from your procedure, if you chose to have throat spray, you will be offered a cold drink when the sensation in your throat has returned to normal.
If you have received sedation, it usually takes about 30 minutes for the initial effects of sedation to wear off although some people may feel fully alert immediately after the procedure, while you recover your oxygen levels, blood pressure and heart rate will be monitored. However, the drugs remain in your blood system for up to 24 hours and you can intermittently feel drowsy with lapses of memory. You will need someone to escort you home and supervise you for this 24 hour period.
Before you leave the department, your nurse or doctor will explain the findings of your gastroscopy and any medication or further investigations that may be needed; they will also inform you if you require further appointments.
If biopsies were taken, they will need to be sent to the pathology lab for further analysis. It may take up to a fortnight for these results to be available, a copy of the results will be sent to your GP.
Sedation can make you forgetful and you may like to have a family member or friend with you when you are given this information.
What are the risks of the procedure?
Gastroscopy is generally regarded as a very safe test, however as with most medical procedures, there are some risks involved. Your doctor will have considered these risks and felt that the benefits of this procedure outweigh the potential risks before they suggested that you should have it carried out.
You need to be aware of the following problems which may arise:
- You may experience bloating and abdominal discomfort for a few hours after the procedure because air is used to inflate the stomach. This can often be relieved by belching.
- You may have a sore throat for 24-48 hours. You must tell the nurse if you have any loose teeth, caps or crowns as there is a risk that they can become dislodged during the procedure.
- If you choose to have sedative drugs, these can cause your breathing to slow down or result in a fall in your blood pressure. This is the reason we do not give high doses of the drugs for the procedure. We monitor your breathing and oxygen levels carefully throughout and this rarely becomes a problem. In any case, an antidote to the sedative drugs that we use is always available and this can reverse its effects immediately.
- There is a risk of causing bleeding at the site of biopsies, but this is uncommon, usually minor and usually stops on its own. Rarely, bleeding may necessitate a blood transfusion or further procedures to stop the bleeding.
- There is a risk of causing a tear (otherwise known as a perforation) in the gullet or stomach with the telescope. This risk is very small and can occur in 1 in 5,000 cases.
If the bowel preparation has not been effective and there is still stool in your bowel, it can hide abnormalities which can be missed. In this event we may need to rebook your procedure with a different bowel preparation.
If you are worried about any of these risks, please speak to your doctor or a member of the team before your test.
Are there any alternatives?
A test known as barium swallow and meal is an alternative to gastroscopy. This is an x-ray examination of the upper digestive tract and can provide similar information to a gastroscopy. However, there are some disadvantages:
- Direct views of the lining of your digestive tract with a gastroscope can provide more information
- Biopsy samples cannot be taken
- The test involves x-ray radiation
If you have questions regarding this alternative test, please ask your doctor.
What is a flexible sigmoidoscopy?
This is an examination of the left half of your large bowel (otherwise known as the large intestine or the colon).
The Endoscopist uses a flexible sigmoidoscope or its longer counterpart, the colonoscope for this procedure. This is a long flexible tube which is about the same thickness as your little finger, it lights up the lining of your large bowel and has a sensor on the end to capture video images which are relayed back to a television screen in the room.
During the investigation, the endoscopist may need to take some tissue samples, known as biopsies, from the lining of large bowel for further analysis. This is completely painless. Photographs may also be taken for your medical records.
Why do I need to have a sigmoidoscopy?
There are a number of reasons why this test may be recommended and your doctor will discuss these with you. Common indications for a colonoscopy include:
- A change in your usual bowel habit to constipation or diarrhoea
- Bleeding from the back passage
- A review of a known bowel condition (e.g. inflammatory bowel disease, colonic polyps)
- To assess or treat an abnormality seen on other tests such as barium enema or CT scan
If none of these apply to you, your doctor will explain any other reasons there may be for having this test.
Will I receive sedation?
Flexible sigmoidoscopy is a short test and most people will remain comfortable without sedative drugs or pain killers. If you are particularly anxious about the test, we can provide intravenous sedation or Entonox gas.

Sedative drugs can be administered into a vein in your arm which will make you drowsy and relaxed for the gastroscopy.
These drugs will NOT make you unconscious like a general anaesthetic. You will be in a state known as cooperative sedation, which means that, although drowsy, you will still be able to hear what is said to you and will be able to follow simple instructions during the investigation, sometimes sedation can also prevent you from remembering anything about the procedure afterwards.
Your oxygen levels and heart rate will be monitored during the procedure, and your blood pressure may also be recorded. You will receive oxygen by small tubes which rest just below your nose.
If you choose to have sedation, you must arrange for a friend or relative to collect you from the Endoscopy Unit and we recommend that they stay with you afterwards. You must not drive, ride a bike, operate machinery, climb ladders, or sign important documents for 24 hours following sedation.
If you are not able to make these arrangements, we will not be able to give you sedation.
Entonox gas

Entonox is a colourless and odourless gas comprised of oxygen and nitrous oxide (commonly known as laughing gas). It is the same gas used by pregnant women during labour pains. It can also be beneficial during flexible sigmoidoscopy and colonoscopy because it helps to relieve pain and has a calming effect.
The gas is administered by a special mouth-piece which you will be asked to hold yourself during the procedure. A two-way valve system allows you to breathe normally through the mouth-piece. The Entonox gas begins to work within 30 seconds and you may feel slightly light headed and sleepy. You can control the amount of gas that you receive yourself by simply removing the mouth-piece but your nurse will monitor you closely throughout the procedure.
One of the benefits of Entonox is that once your procedure is over, the gas is rapidly eliminated from the body and you are usually safe to leave the department soon afterwards. Unlike with intravenous sedation, you are permitted to drive just 30 minutes after the test as long as you feel back to your normal self.
Entonox is very safe in the majority of people. It can cause mild nausea, dizziness and a dry mouth. As the effects of the drug wear off very quickly, so do these side effects. Please be aware that Entonox may not be suitable for you if you have respiratory conditions such as COPD, severe bullous emphysema or a collapsed lung.
How to prepare for your sigmoidoscopy?
It is extremely important that the left side of your bowel is completely empty before a flexible sigmoidoscopy to allow adequate inspection of the lining of your colon.
This is usually achieved by giving you a bowel cleansing laxative to take at home on the day before your procedure. Sometimes, an enema on the day of the test is all that is required, you will be informed if this is the case
On our Endoscopy units we usually use a bowel cleansing agent called Moviprep®, you should have been provided with this medication along with clear instructions on how to administer it. If you have any queries do not hesitate to contact the endoscopy unit and we will be happy to help you.
If you have been told that you will be given an enema for your flexible sigmoidoscopy, it will be given to you shortly before your procedure in the endoscopy department. An enema is a liquid preparation which is squirted into the back passage and induces a bowel movement. This will help to ensure that the left side of your bowel is clear.
What happens when I arrive?
Our reception staff will greet you on the unit; once they have checked your details you will be offered a seat in the waiting room. Your named nurse will ask you to come through to the preparation area shortly before your procedure.
Your Nurse will check your identity and go through any medical conditions, medication and allergies to ensure it is safe to proceed. It would be very helpful if you could bring a list of all your medication with you, your Nurse will also ensure arrangements have been made for your journey home. Your blood pressure and pulse will be checked prior to the procedure.
You will be asked to change into a hospital gown and we can also provide modesty shorts which keep you well covered during the procedure to preserve your dignity.
Please do not bring large amounts of money or valuables with you.
Your Endoscopist will go through your consent form and answer any questions you may have. If you have already signed your consent form, we will confirm that you have not changed your mind.
If you have decided to have sedation, a plastic tube, known as a cannula will be inserted into a vein in your hand or arm to allow the drugs to be injected.
What happens during the procedure?
The sigmoidoscope is introduced into the back passage and maneuvered around the left side of your large bowel. There are some bends that naturally occur in the bowel and negotiating these may result in brief periods of discomfort.
Air is gently passed into the bowel during the investigation to facilitate the passage of the camera. You may be asked to change position during the test, to help pass the endoscope around your bowel, and the endoscopy nurses will help you move if necessary.
We will ensure that you are well covered up throughout the procedure to preserve your dignity.
Once the sigmoidoscope has been passed around the left side of your bowel, the endoscopist will slowly withdraw the instrument making a close inspection of the lining of your bowel to look for any abnormalities. Some of the air blown into the bowel will be removed as well, which will ensure you remain comfortable.
During the procedure samples, known as biopsies, may be taken from the lining of your bowel for analysis in our laboratories. These will be retained for future tests if they become necessary.
The procedure usually takes about 10 minutes but this can vary depending on how many twists there are in your bowel, and whether any additional procedures are required.
What is a polyp/polypectomy?
A polyp is a small growth that can form on the lining of the bowel. Most polyps are harmless but if they are left to grow, some forms of polyps can develop in to a cancer.
The removal of a polyp is called a polypectomy and is performed by using a variety of instruments through central channels of the endoscope.
If a polyp is found on the left side of your bowel, there is a higher chance of you having polyps on the right side of your bowel. As a flexible sigmoidoscopy does not reach the right side of your bowel, if a polyp is found you may be asked to return on another day for a full colonoscopy this allows the entire large bowel to be examined and any further polyps to be removed.
What happens after the procedure?
You will be escorted to the recovery area in order to rest while you recover from your procedure, if you chose to have throat spray, you will be offered a cold drink when the sensation in your throat has returned to normal.
If you have received sedation, it usually takes about 30 minutes for the initial effects of sedation to wear off although some people may feel fully alert immediately after the procedure, while you recover your oxygen levels, blood pressure and heart rate will be monitored. However, the drugs remain in your blood system for up to 24 hours and you can intermittently feel drowsy with lapses of memory. You will need someone to escort you home and supervise you for this 24 hour period.
If you received Entonox gas during the procedure, its effects usually wear off within a few minutes. You will be observed in the department until you feel back to your normal self.
Before you leave the department, your nurse or doctor will explain the findings of your gastroscopy and any medication or further investigations that may be needed; they will also inform you if you require further appointments.
If biopsies were taken, they will need to be sent to the pathology lab for further analysis. It may take up to a fortnight for these results to be available, a copy of the results will be sent to your GP.
Sedation can make you forgetful and you may like to have a family member or friend with you when you are given this information.
Are there any risks?
Flexible sigmoidoscopy is generally regarded as a very safe test, however as with most medical procedures, there are some risks involved. Your doctor will have considered these risks and felt that the benefits of this procedure outweigh the potential risks before they suggested that you should have it carried out.
- You may experience bloating and abdominal discomfort for a few hours after the procedure because air is used to inflate the stomach. This can often be relieved by belching.
- If you choose to have sedative drugs, these can cause your breathing to slow down or result in a fall in your blood pressure. This is the reason we do not give high doses of the drugs for the procedure. We monitor your breathing and oxygen levels carefully throughout and this rarely becomes a problem. In any case, an antidote to the sedative drugs that we use is always available and this can reverse its effects immediately.
- There is a risk of causing bleeding at the site of biopsies, but this is uncommon, usually minor, and usually stops on its own. Rarely, bleeding may necessitate a blood transfusion or further procedures to stop the bleeding.
- There is a risk of causing a tear (otherwise known as a perforation) with the telescope. This risk is very small and can occur in 1 in 2000 cases.
- Sigmoidoscopy is not a perfect test, whilst we normally will get excellent views, there is a small risk (between 5-10%) that we can miss pathology during your procedure due to the number of bends and folds that are in the bowel and the quality of the bowel preparation. You will be advised that if your symptoms persist or if you develop any new symptoms, you should seek medical advice.
If the bowel preparation has not been effective and there is still stool in your bowel we may need to rebook your procedure with a different bowel preparation.
Are there any alternatives to a flexible sigmoidoscopy?
An X-ray test (barium enema) or a CT scan (CT virtual colonoscopy) can be used to look at your large bowel, the main drawback of these tests is that they only provide pictures of the shape of your bowel and do not allow samples to be taken or any polyps to be removed. You would require a similar bowel preparation for these tests as well.
Your doctor will have considered a barium enema or CT virtual colonoscopy for you before asking you to have a flexible sigmoidoscopy.
If you do have questions about these alternatives, please mention them to your doctor.